Explained: What is Avascular Necrosis, the latest post-COVID condition
Doctors dealing with such AVN cases say after mucormycosis this can be the next worrying trend in recovered patients
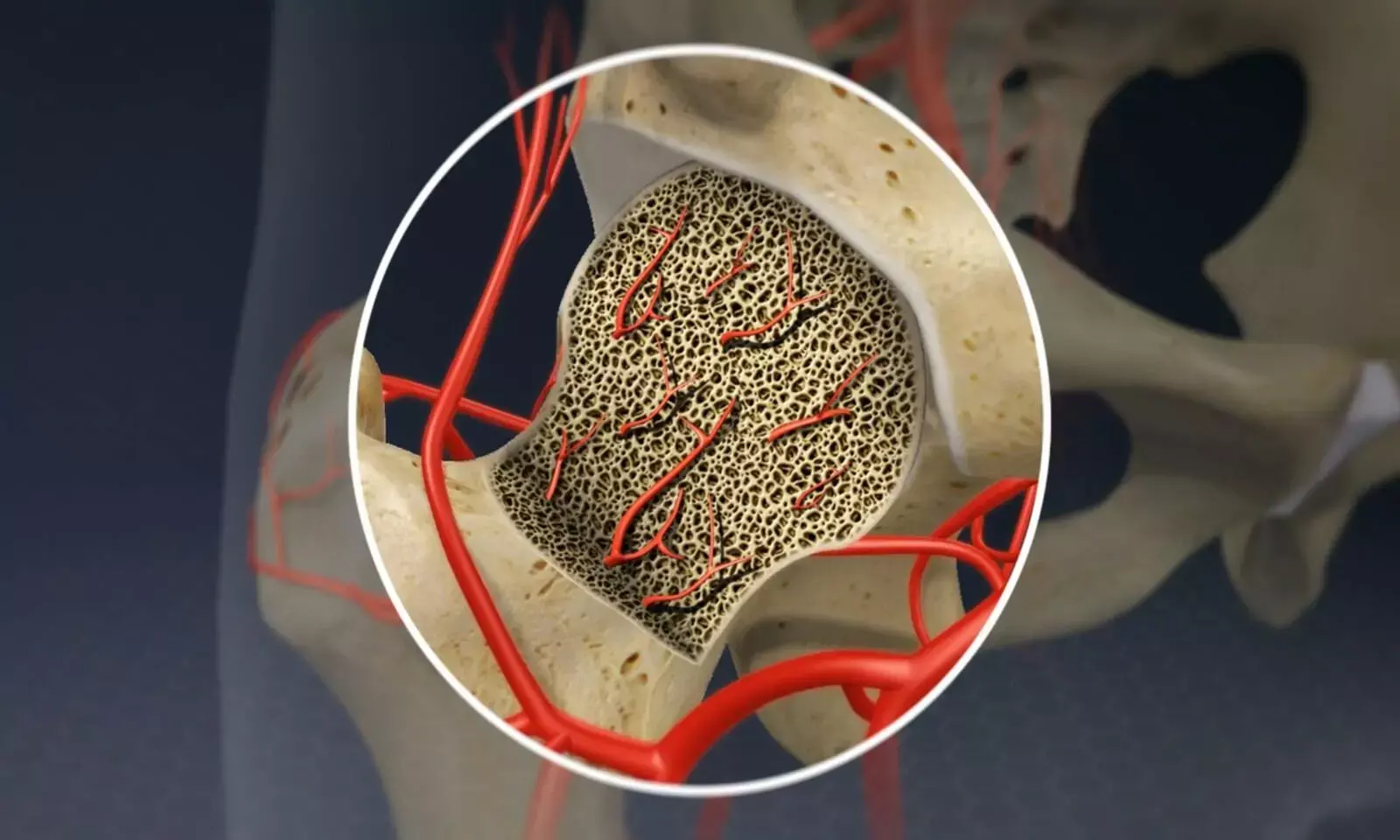
Image Source: Johns Hopkins Medicine (Osteonecrosis of the hip)
The second wave of COVID-19 in India saw more and more cases of complications in recovered COVID patients, such as mucormycosis, blood clots, new onset diabetes, chronic fatigue among others. The latest is Avascular Necrosis (AVN) or Osteonecrosis. Doctors in Mumbai's PD Hinduja Hospital recently reported at least three cases of AVN and a day later, Delhi's BLK Super Speciality Hospital reported three more.
In common parlance, it is the 'death of bone tissue due to lack of blood supply'. In detail, AVN is a degenerative bone condition which existed way before COVID-19. But doctors think this could be the next worrying trend in post-COVID complications. To know more, FactChecker spoke to two specialists: Dr Sanjay Agarwala, head of orthopaedics at PD Hinduja Hospital and the doctor treating the three Mumbai patients, and Dr Gauresh Palekar, an orthopaedic surgeon at Jaslok Hospital in Mumbai.
Avascular Necrosis and its causes
Avascular Necrosis is a disease that occurs when the blood supply to the bone is temporarily or permanently cut off, according to Johns Hopkins University School of Medicine. This most commonly affects the ends of a long bone leading to small breaks in the bone and causes the bone's eventual collapse. It may affect one bone, several bones at one time, or different bones at different times. But most often it affects the hip.
"The cells in the femoral head (highest part of the thigh bone) die. One of the reasons is loss of blood supply, others are mostly due to steroids, alcohol and sickle cell disease. This can cause avascular necrosis," Dr Palekar told FactChecker.
"The patient will complain of pain around the hip or the groin region. It could make it very difficult to walk which could lead to limping in the patient. There is also severe pain around the knee joint, in the lower back and groin making their mobility very difficult. After the onset of COVID-19 the frequency of this disease has been growing rapidly and after mucormycosis it could be one of the biggest challenges," added Dr Palekar.
According to Dr Agarwala, referring to this disease as 'bone death' (term used by several news reports) is a bit dramatic. Avascular means that there is no blood whereas necrosis means death of cells. This phenomenon, which was described in the 1960s, is seen most commonly in the hip and it's got two unique features: one, it is weight bearing in the joints and the second is that they are hairpin blood vessels which have a greater propensity to block off, said the Hinduja doctor.
Both doctors said they deal with about seven to eight cases of AVN a week. "I deal specifically with this disease so this may not be a representative figure for most orthopaedic surgeons," said Dr Palekar.
Doctors have observed a sudden rise in AVN cases during the COVID-19 second wave. "We used to have around five AVN patients in a week, but suddenly the number is growing. The commonality here was that they were all survivors of COVID-19. All these patients were receiving life-saving steroids," said Dr Agarwala.
Not all patients on steroids will develop AVN as it occurs in only those who are sensitive to certain steroids or those who have a predilection for developing AVN.
AVN can also be caused by traumatic events such as a fracture, dislocation of joints or during cancer treatment due to exposure to radiation. Alcohol or steroid abuse are also major risk factors. "AVN has been there for quite some time. This disease takes a while to come to the fore unlike mucormycosis. It commonly affects people in the 30-50 years age group; more common in males than females, but it can affect younger or older people," said the doctor from Jaslok Hospital.
"Around 20 years ago, a patient with AVN came to me with severe hip pains. I immediately admitted him and recognised that the bone had become soft like a boiled potato because of avascularity. If this happens in the heart, you have a heart attack, in the brain you might have a stroke. In this case, you get a sector necrosis since blood supply has stopped. So, if there is pressure on that bone that bone collapses," explained Dr Agarwala.
How has COVID-19 caused a rise in AVN cases?
The medical cohort is still researching the implications of COVID-19, said the doctors. Although the exact reason is still unknown, there is a possible chance that medicines taken during COVID treatment could have reduced blood flow in the body.
"It has not been proven until now. But as we know, COVID affects blood vessels and causes clotting. It is in a hypercoagulable state where spontaneous clots happen at multiple places in the body. So, the connection between COVID-19 and AVN is maybe via steroids but there can be a direct connection as well where there is an intravascular blood clot causing the femoral head's death but up till now nobody has come up with a concrete reason for this," said Dr Palekar.
Dr Agarwala and his colleagues at PD Hinduja Hospital have recently published a paper in The British Medical Journal titled 'Avascular Necrosis as part of Long COVID-19' where they've explained that the large-scale use of Corticosteroids in COVID-19 cases is expected to trigger a resurgence of AVN in post-COVID patients. However, the doctor believes this should not be an excuse to not take medicines prescribed for COVID-19.
When asked if patients with arthritis were prone to AVN, both doctors said that arthritis was generic for a host of diseases and hence they are not prone to this disease.
Diagnosis and treatment
According to Dr Agarwala, in India, the Indian Society of Hip and Knee Surgeons (ISHKS) were the first to recognise that there should be a registry of patients who need a hip replacement. "In India, 50% of cases which need hip replacement have had an antecedent of AVN," he said.
However, there are limited studies in this area in Indian population. According to a 2018 study published in the Indian Journal of Orthopedics, titled 'Epidemiological Profile of Femoral Head Osteonecrosis in the North Indian Population', steroid administration (37.3%) was the most commonly observed cause among the study's 249 Indian patients, followed by chronic alcohol intake (20.1%) and trauma (15.3%).
AVN can be classified into four stages. In Stage 1, you can only see it on MRIs and bone scans. In Stage 2, you can start seeing it on X-rays. In Stage 3, it starts collapsing and in the last stage, you need a hip replacement. "If you've reached the third stage, you're probably missing the bus. If you start thinking about it in the first two stages, you have a medical line of cure," said Dr Agarwala.
Both doctors stressed on the need of diagnosing the disease early. "It has to be diagnosed at the correct time. If you diagnose AVN early, it can be treated but if it is diagnosed at a later stage, the person may have to undergo a joint replacement. Hence, MRI is very important to identify the disease," explained Dr Palekar.
To delay the progress of degeneration in the bones, pharmacological treatment is recommended in the early stages of AVN. These medicines cost approximately Rs 500 per month. Different surgical treatments are also suggested for the first two stages such as core depression and osteotomy. This helps increase blood flow to the bone.
In the last stage, the only option is hip replacement wherein the damaged bone is removed and replaced with prosthetics.
In the case of a post-COVID patient, on early suspicion after complaints of hip and thigh pain, diagnosis can be established by early MRI and can be successfully treated with bisphosphonate therapy, concluded Dr Agarwala.


