How to Prepare for the "Unavoidable" Third Wave of COVID-19?
Boost public health workforce, scale up vaccination and prepare robust healthcare plan for this emergency, say experts
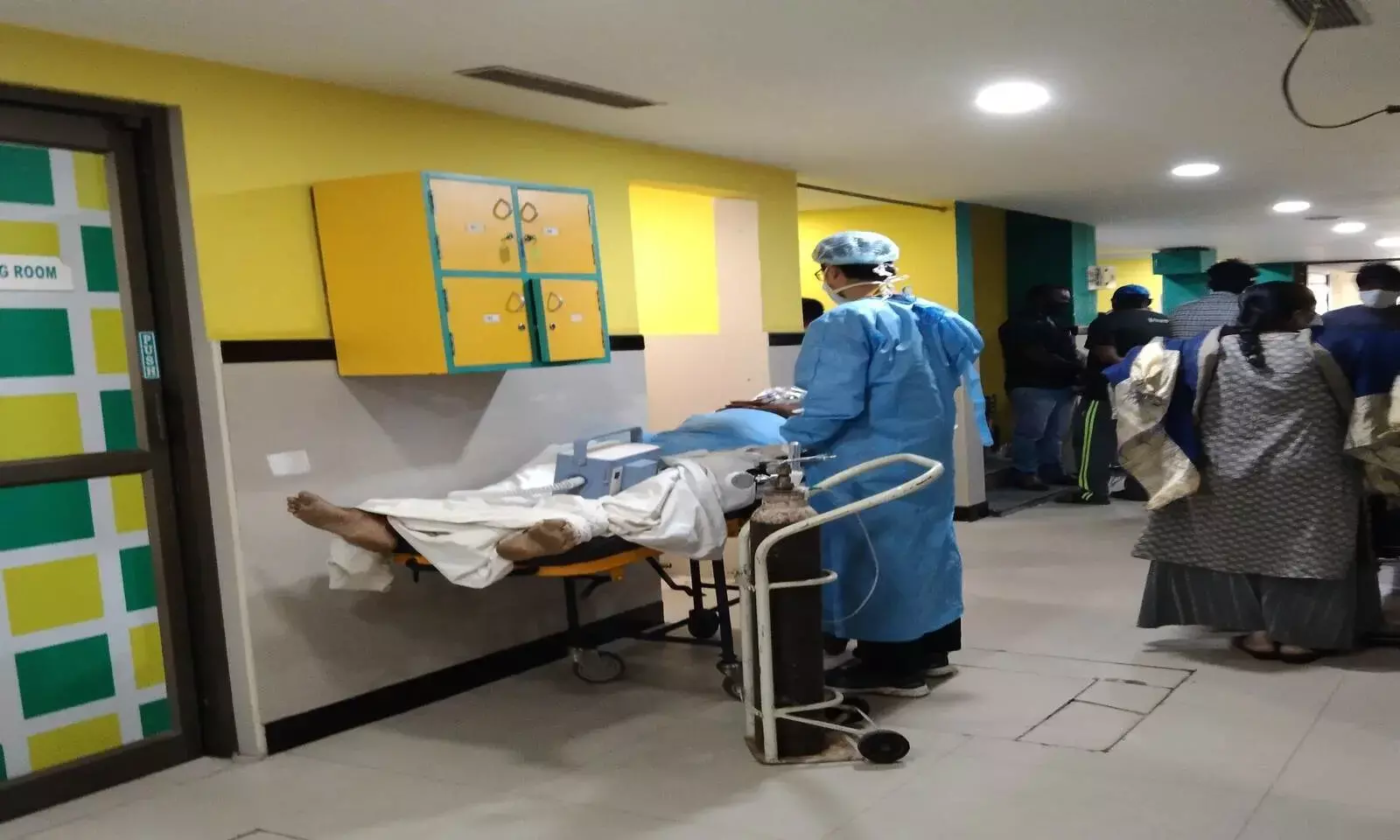
Photo: Nidhi Jacob
India is reeling under the second wave of COVID-19, for which it was infrastructurally and resource-wise unprepared for. The country reported more than four lakh cases on April 30, 2021, becoming the first country in the world to cross the four-lakh mark. And healthcare experts are already predicting that there'd be a third wave.
Dr Devi Shetty, noted cardiac surgeon and chairman, Narayana Health, recently said India should be prepared for a third wave and he suggested some solutions too. "The current pandemic is likely to last for about 4 to 5 months. And then we should be prepared for the third wave," said Dr Shetty in an online address at the Symbiosis Golden Jubilee Lecture Series.
Also, Maharashtra Chief Minister Uddhav Thackeray told the state government to be prepared for a third wave of COVID-19 in July or August this year.
So, FactChecker asked three public health experts what it is that they suggest India does to brace for the next wave. The responses ranged from strengthening the public healthcare workforce to a better supply chain and planning.
Health workforce
In August 2020, the Indian Medical Association President Dr Rajan Sharma wrote to Prime Minister Narendra Modi demanding a national solatium for doctors. In the letter, he also cited that 87,000 healthcare workers were infected with the virus and 573 had died, according to government's data. In April 2021, a state-wise analysis by IMA showed that 747 doctors in the country died of COVID-19.
"We need to produce at least two lakh nurses and at least one and a half lakh doctors in the next few weeks who are dedicated to managing COVID for the next one year," said Dr Shetty.
He suggested that the Ministry of Health along with the Indian Nursing Council consider nursing students (General Nursing and Midwifery) as graduates, and deploy them to work in COVID ICU wards for one year.
Dr Shahid Jameel, virologist and director of the School of Biosciences at Ashoka University, seconded Dr Shetty and said, "We should never again be caught with inadequate infrastructure (hospitals and doctors/HCWs), poor supply chains (medicines, oxygen, etc) and most importantly, shoddy planning."
On May 3, 2021, the Centre announced key decisions to boost availability of medical personnel to fight COVID-19. One of the main decisions is to prioritise medical personnel completing 100 days of Covid duty and to give them priority in forthcoming regular government recruitments. It has also been decided to deploy medical interns in COVID-19 management duties under the supervision of their faculty.
"The shortfall of doctors is about 33%, nurses 45%, beds 75%. So, our healthcare had been working sub-optimally even before the pandemic. While most modern nations have virtually eliminated the classical tropical infectious diseases, in India, such diseases clutter the healthcare institutions making even the time available for doctors per patient woefully just a few minutes only," Dr T Jacob John, virologist and former professor at the Christian Medical College, Vellore told FactChecker.
"Moreover, doctors are not distributed evenly. Five states with 30% of the total population have 50% doctors, leaving the rest of India grossly under-served," Dr John added.
Highlighting how the well-being, especially mental health, of those who see so much sickness and death is also important, Jameel said that if they are overworked, the quality of care goes down, which pushes up mortality.
He suggested that to address this, the government should bring in retired doctors/healthcare workers and also deploy dentists, pharmacists and those training in alternative systems of medicine such as Unani and Ayurveda be given a short training in critical and supportive care. This would take the workload off those who are needed to care for the severely ill, explained Jameel.
Scaling up vaccination
India began its phased vaccination programme on January 16, 2021 targeting 300 million people. It was designed to first immunise vulnerable populations based on evidence from the first wave. This included nearly 10 million healthcare, 20 million frontline workers and 270 million people above the age of 50 (those with or without comorbidities).
India has also exported about 64 million vaccine doses to 70 countries. According to a United Nations (UN) spokesperson, on April 28, 2021, India turned down UN's offer of assistance from its integrated supply chain saying it has its own "robust" system to manage the logistics of getting material for dealing with the COVID-19 surge.
As on May 5, 2021, India has administered more than 16 crore vaccine doses in the country of which more than 13 crore were administered as first dose and over 3 crore as second dose.
"Vaccines are powerful tools. While vaccines would no longer help contain the current second wave because they take 6-8 weeks to show protection, they will reduce the intensity of future outbreaks," said Dr Jameel.
"The task, therefore, is to vaccinate as many people as quickly as possible. This requires proper planning to ensure adequate supplies, delivery points and effective communication. Unfortunately, for reasons of hesitancy and poor communication, we lost valuable time in January and February when the daily caseload was reducing. Now, it is an uphill battle," he added.
Dr Giridhar Babu, professor and head of Life Course Epidemiology at the Public Health Foundation of India told FactChecker that a combination of high vaccine coverage and mitigation measures can prove helpful.
"If we vaccinate a significant proportion of people and if we are careful about preventing it from the beginning then we could reduce the severity of the disease. Vaccination coupled with control measures such as containment and mitigation strategies can prevent the third wave from being worse than the first two," he said.
Pandemic preparedness and mitigation plan
Any temporary measure is futile without having a robust public health care system, say public health experts. Dr John said we need to think politically about health.
"We failed to plan and failed to meet the needs. India must shift national policy and establish universal healthcare, primary, secondary and tertiary without any more loss of time. The ruling party has the necessary majority to get reforms through rapidly. The Ruling government's party must call all party meetings for consensus for spending 10% GDP, on health, on an expanding time schedule. Half of that must be for establishing public health which we have neglected for more than 70 years," the Vellore-based virologist explained.
Another highlight is not forgetting health and wellness centres in urban areas. The PHFI professor suggested that there should be at least one such centre per 5,000 people with additional doctors and nurses in urban areas to promote primary healthcare so people don't have to rely on costly health services.
"When there is an earthquake, we have a disaster mitigation plan. But in a pandemic, we still don't have a robust plan in dealing with a health emergency," said Dr Babu.
"This crisis cannot be dealt with by increasing the capacity of health workers alone. We can't create four to five lakh workers just like that. Hence, we need to redistribute and use our complete workforce. This will not end with the third wave in India and therefore the day when the cases start rising we need to immediately plan on imposing lockdowns, reduce movement and use the workforce in an efficient manner. We should not be caught by surprise again," he added.
Can a COVID-19 third wave be prevented?
When asked this, experts told FactChecker that a third COVID-19 wave is unavoidable but that it can be delayed and reduced in severity.
"Based on what we have seen so far, a third wave is unavoidable. But we cannot say if it would be better or worse than the current one. That will depend upon how many people get infected and vaccinated during the next few months. The severity will depend also on how prepared we are with medical infrastructure and supply chains," said Dr Jameel.
He highlighted how the severity of this wave is not because the virus has become more lethal, but because it has become more infectious and transmissible. And a solution to it is tracking emerging viral variants that can compromise preparations.
"We know and can deal with what is currently contributing to the second wave. But more infectious and/or more lethal variants can easily change the future course. For this, it is important to sequence viruses in the population at sufficient density, and pay attention to what is emerging," Dr Jameel ended.


